June 29, 2018
Antidepressant could be promising treatment for a serious liver disease, UCalgary research study discovers

Gail Wright considered herself healthy. She had no idea she had a chronic liver disease. “I was at a routine check-up and my doctor said my liver enzymes were elevated. I was sent to a specialist but I wasn’t too worried. I didn’t have any symptoms.”
She soon learned she had primary biliary cholangitis (PBC), a rare, incurable liver disease which can be fatal if untreated. PBC is more commonly diagnosed in women, usually between the ages of 40 and 60. Symptoms can include severe fatigue and itchiness. Wright has responded well to the typical treatment (ursodeoxycholic acid) but 30 per cent of patients don’t respond well. For them, the autoimmune disease can have serious complications that may lead to a liver transplant. PBC is the second-leading cause of liver transplant in Canada.
A team of scientists at the University of Calgary’s Cumming School of Medicine (CSM) discovered what could be a new option for these hard-to-treat patients. A drug usually prescribed for depression appears to effectively stop progression of PBC. Dr. Abdel Aziz Shaheen, MD, a gastroenterologist and epidemiologist, was researching the effect of depression on people with PBC and came upon an unexpected finding. While he was combing through the data, he found a sub-group of people with depression who were healthier than the others.
“At first, I thought I must have an error in my coding. As I began to look deeper I realized these patients were all taking the antidepressant mirtazapine, which seemed to be having a positive impact on their liver disease,” says Shaheen, an assistant professor in the departments of community health sciences and medicine and member of the CSM’s O’Brien Institute for Public Health. “You don’t expect to find people with a chronic illness and depression to be healthier than those patients who don’t have depression.”
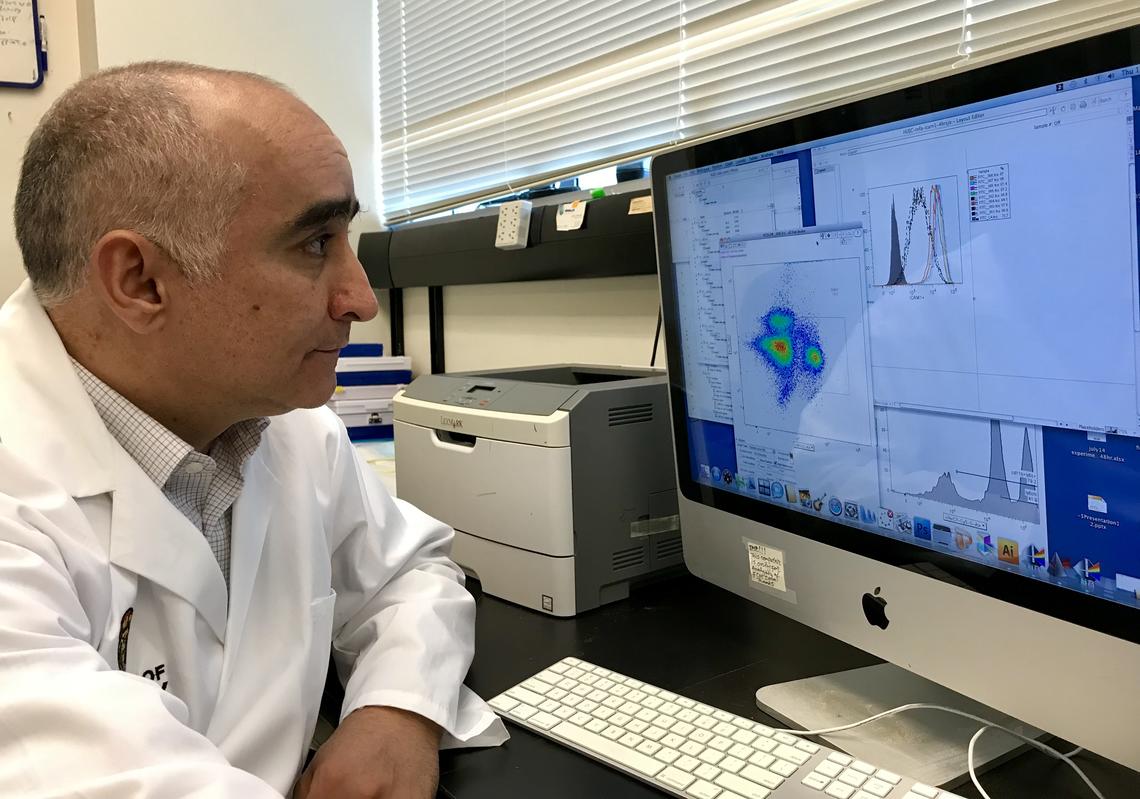
Wagdi Almishri is doing research in Swain’s lab to determine how mirtazapine can benefit the liver.
Kelly Johnston, Cumming School of Medicine
Shaheen was eager to investigate further so he recruited colleagues from the Department of Psychiatry and basic scientists to study what might be happening inside the body that would lead to this result. Dr. Mark Swain, MD, a liver specialist, clinician scientist and member of the Snyder Institute for Chronic Diseases began looking at mouse models to learn how the antidepressant was affecting the liver.
“PBC slowly destroys the small bile ducts of the liver. Once damaged, the liver can 'fill up' with materials the body is trying to excrete, damaging the liver and leading to permanent scarring,” says Swain, who is head of the Division of Gastroenterology and Hepatology in the Department of Medicine, and holds the Cal Wenzel Family Foundation Chair in liver disease. “Mirtazapine has significant effects on the immune system which appear to be protective to the liver.
“No one thought that an antidepressant could affect liver immunity,” says Swain. “This leads to an entire new line of inquiry, on how antidepressants may be used in the treatment of other chronic diseases.”
“This confirms how important collaboration is in the field of medicine. We are very lucky at the University of Calgary to be able to reach out to our colleagues in other institutes and departments to help solve mysteries to improve patient care,” says Shaheen. “I couldn’t have explained this finding alone.”
Postdoctoral fellow Wagdi Almishri is doing ongoing research in Mark Swain’s lab to determine how mirtazapine has a beneficial effect on the liver in primary biliary cholangitis patients. The findings from this research work may have important implications for improved treatment for a broad range of other chronic autoimmune diseases.
The Canadian Institutes of Health Research Institute of Nutrition, Metabolism and Diabetes is proud to have supported this research work. Findings are published in PLOS ONE.
